
Are you experiencing a lichenoid drug eruption caused by hydrochlorothiazide medication?
Don’t worry, we are here to help!
Our specialized treatment can provide relief and bring back the health of your skin!
At our clinic, we understand the discomfort and frustration that comes with lichenoid drug eruption. Our team of dermatologists and experts are dedicated to providing you with the best possible care and treatment options.
With our innovative and personalized approach, we can help you manage and alleviate the symptoms of lichenoid drug eruption caused by hydrochlorothiazide.
Don’t let your skin condition hold you back. Contact us today and schedule an appointment to start your journey towards healthier skin!
What is Lichenoid Drug Eruption?
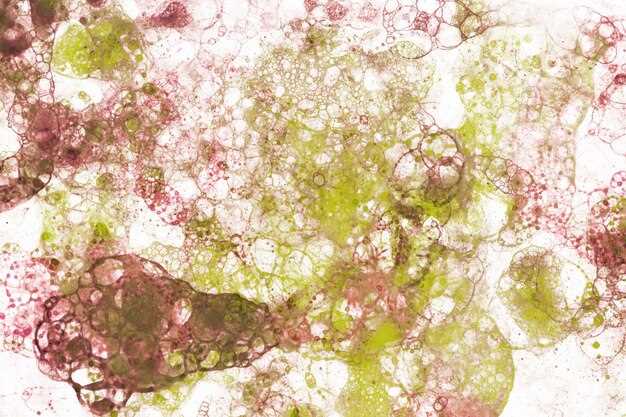
Lichenoid drug eruption is a type of skin reaction that occurs as a response to certain medications. It is characterized by the presence of lichenoid papules or plaques on the skin. These lesions usually have a symmetrical distribution and can be itchy or painful.
Common medications that can cause lichenoid drug eruption include certain antibiotics, antihypertensive drugs, nonsteroidal anti-inflammatory drugs, and diuretics. The exact mechanism behind the development of lichenoid drug eruption is not fully understood, but it is thought to involve an immune-mediated response.
Symptoms of Lichenoid Drug Eruption
The symptoms of lichenoid drug eruption can vary from person to person, but common signs include:
- Red or purple papules or plaques on the skin
- Itching or pain in the affected area
- Lesions that are flat or raised
- Symmetrical distribution of the lesions
In some cases, lichenoid drug eruption may also cause blisters or ulcerations on the skin. It is important to note that the symptoms can take several weeks to develop after starting a new medication.
If you suspect that you may have lichenoid drug eruption, it is important to consult with a healthcare professional for an accurate diagnosis and appropriate treatment.
Treatment Options for Lichenoid Drug Eruption
When it comes to treating lichenoid drug eruption, there are several options available to help alleviate the symptoms and promote healing. It is important to consult a healthcare professional before starting any treatment.
- Discontinuation of the Offending Drug: The first and most crucial step in treating lichenoid drug eruption is identifying and discontinuing the medication responsible for the reaction. This may involve consulting with a healthcare provider.
- Topical Corticosteroids: These medications are commonly prescribed to reduce inflammation and itching associated with lichenoid drug eruption. They can be applied directly to the affected areas of the skin to provide relief.
- Systemic Corticosteroids: In more severe cases, oral or injectable corticosteroids may be prescribed to help control the immune response and reduce inflammation throughout the body.
- Immunosuppressive Medications: In certain instances, immunosuppressive drugs may be recommended to suppress the immune system’s response and manage the symptoms of lichenoid drug eruption.
- Phototherapy: Light therapy, such as narrowband ultraviolet B (NB-UVB) therapy, may be used in some cases to improve the symptoms of lichenoid drug eruption. This treatment involves exposing the affected skin to controlled amounts of UVB light.
- Supportive Care: In addition to specific treatment options, it is important to provide supportive care to the affected individual. This may include keeping the skin clean and moisturized, avoiding irritants or triggers, and taking steps to relieve itching and discomfort.
Remember, these treatment options are only general recommendations and may vary depending on the individual and the severity of the lichenoid drug eruption. It is best to consult with a healthcare professional for a personalized treatment plan.
Treatment Options for Lichenoid Drug Eruption
Preventing Lichenoid Drug Eruption is essential to avoid discomfort and further complications. Here are some treatment options to consider:
1. Discontinuation of the Medication
The first step in managing Lichenoid Drug Eruption is to discontinue the medication that is causing the eruption. This involves consulting a healthcare professional who can help identify the specific drug responsible for the condition. Once the medication is discontinued, the symptoms of the eruption usually begin to improve.
2. Topical Steroids
Topical corticosteroids, such as hydrocortisone creams or ointments, can be applied to the affected areas to reduce inflammation and relieve itching. These medications are available over-the-counter or may be prescribed by a healthcare professional. It is important to follow the instructions for use and consult a healthcare professional if the symptoms do not improve or worsen.
3. Systemic Steroids

In some cases, when the eruption is severe or does not respond to topical treatments, systemic steroids may be necessary. These are prescription medications that are taken orally or administered through injections. Systemic steroids work by suppressing the immune response and reducing inflammation throughout the body. However, they may have side effects and should be used under the guidance of a healthcare professional.
4. Immune Modulating Medications
In certain cases, immune modulating medications may be prescribed to manage Lichenoid Drug Eruption. These medications help regulate the immune system and reduce the inflammatory response. Examples of immune modulating medications include methotrexate and azathioprine. These medications are generally prescribed for severe cases or when other treatment options have not been effective.
5. Symptomatic Relief
In addition to the above treatments, symptomatic relief measures can be taken to manage the discomfort associated with Lichenoid Drug Eruption. These may include over-the-counter pain relievers, antihistamines, and soothing creams or lotions. It is important to consult a healthcare professional before using any over-the-counter medications to ensure they do not interfere with other prescribed treatments.
| Advantages | Considerations |
|---|---|
|
|
Remember, it is important to consult a healthcare professional for an accurate diagnosis and personalized treatment plan for Lichenoid Drug Eruption. Early intervention and appropriate treatment can help manage the condition effectively and prevent future occurrences.
Preventing Lichenoid Drug Eruption
To prevent lichenoid drug eruption, it is important to be cautious when taking medications that have been known to cause this condition. Here are some steps you can take to minimize the risk:
- Inform your healthcare provider about any previous episodes of lichenoid drug eruption or any known allergies.
- Read the medication labels and package inserts carefully to identify any potential side effects or warnings related to lichenoid drug eruption.
- Avoid medications that have been associated with lichenoid drug eruption, if possible.
- If alternative medications are not available, discuss the risks and benefits with your healthcare provider before starting the medication.
- Follow the prescribed dosage and frequency of the medication closely.
- If you experience any unusual symptoms or skin changes while taking the medication, promptly notify your healthcare provider.
- Avoid exposure to other potential triggers, such as certain foods, chemicals, or environmental factors, that may increase the risk of lichenoid drug eruption.
- Maintain good overall health and hygiene practices to support the body’s immune system and minimize the risk of lichenoid drug eruption.
- Consider seeking a second opinion if you have concerns about the prescribed medication or treatment plan.
- Regularly follow up with your healthcare provider to monitor any potential side effects and discuss any necessary adjustments to your medication regimen.
- By being proactive and informed, you can play an active role in preventing lichenoid drug eruption and promoting your overall health and well-being.
Causes of Lichenoid Drug Eruption
Lichenoid drug eruption is a skin condition that occurs as a result of an allergic reaction to certain medications. Various drugs have been associated with the development of lichenoid drug eruption, including:
- Antihypertensive medications, such as hydrochlorothiazide and ACE inhibitors.
- Nonsteroidal anti-inflammatory drugs (NSAIDs), like ibuprofen and naproxen.
- Antibiotics, such as penicillin and tetracycline.
- Anticonvulsant medications, including phenytoin and carbamazepine.
- Cardiovascular drugs, like beta-blockers and calcium channel blockers.
It is important to note that not everyone who takes these medications will develop lichenoid drug eruption. Some individuals may have a higher susceptibility to this type of allergic reaction, while others may not experience any adverse skin effects at all. The exact cause of lichenoid drug eruption is still not fully understood, but it is believed to involve an immune response triggered by the medication.
If you suspect that you may be experiencing lichenoid drug eruption or have any concerns about your medication, it is important to consult with a healthcare professional for an accurate diagnosis and appropriate management options.
